Sexual Health – Genital Warts
Genital Warts
Human Papilloma Virus (HPV)
Introduction
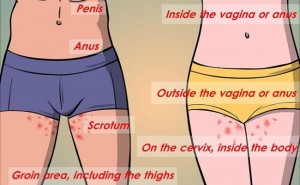
Genital warts are small fleshy growths, bumps or skin changes that appear on or around the genital or anal area.
Genital warts are very common. In England, they are the second most common type of sexually transmitted infection (STI) after chlamydia.
Genital warts are the result of a viral skin infection caused by the human papilloma virus (HPV). They are usually painless and do not pose a serious threat to health.
But they can be unpleasant to look at and cause psychological distress.
There is no evidence that your fertility will be affected by genital warts.
The human papilloma virus (HPV)
The HPV is not a single virus, but a family of more than 100 different strains of viruses. Different strains usually affect different parts of the body, including the hands or feet.
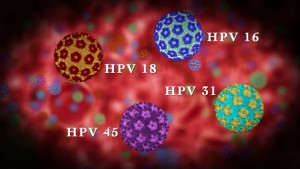
Although around 30 different types of HPV can affect the genital skin, most cases of infection with HPV cause no visible symptoms. Around 90% of all cases of genital warts are caused by two strains of the virus type 6 and type 11.
The types of HPV that cause visible genital warts do not cause genital cancer. Other strains of HPV can cause cervical cancer.
How do they spread?
Genital warts can be spread during vaginal or anal sex, and by sharing sex toys. But you don’t need to have penetrative sex to pass the infection on because HPV is spread by skin-to-skin contact.
It can take months, or even years, for warts to develop after infection with HPV. So if you’re in a relationship and you get genital warts, it does not necessarily mean your partner has been having sex with other people.
HPV is most likely to be transmitted to others when warts are present, although it is still possible to pass the virus on before the warts have developed and after they have disappeared.
*Condoms do not provide complete protection because it is possible for the skin around your genital area not covered by the condom to become infected.
Treating genital warts
If you think you have genital warts, see a health professional as they may need to be treated. It is possible to have more than one STI at a time, so if you think you have warts, it is a good idea to have a check-up.
You can make an appointment at your local sexual health or genitourinary medicine (GUM) clinic.
You can go to a sexual health clinic whatever age you are. If you’re under 16, the service is still confidential and the clinic won’t tell your parents. Find your local sexual health or GUM clinic.
The treatment for genital warts depends on how many warts you have and where they are. Several treatments are available, such as liquids or creams and freezing the warts (cryotherapy).
*You should not use wart creams that are available over the counter because they are designed to only treat warts on the hands or verruca’s.
If you are diagnosed with genital warts, it is recommended you do not have sex, including anal and oral sex, until your genital warts have fully healed. This will help prevent you passing the infection on to others. It will also help speed up your recovery.
Will the warts come back?
Some people only ever get one episode of genital warts. For many others, the warts will come back weeks, months or years later.
If you do develop a new wart, it is not possible to say if these are a result of the original infection or a new infection with HPV.
Who is affected?
Both men and women can be affected by genital warts. According to Public Health England, in 2012 there were 73,893 new cases of genital warts diagnosed by GUM clinics in England. This compares with 206,912 new cases of chlamydia in 2012.
Genital warts are most common in sexually active teenagers and young adults. The highest rates of genital warts occur in men aged 20 to 24 years and women aged 16 to 19 years.
HPV vaccinations
HPV vaccines in the UK are offered to all girls in year 8 (aged 12 to 13 years).
Since September 2012, the vaccine Gardasil has been used and can help protect against HPV types 6 and 11, which cause around 90% of genital warts. It also protects against types 16 and 18, which are linked to more than 70% of cases of cervical cancer in the UK.
Before September 2012, a different vaccine called Cervarix was used to protect against HPV types 16 and 18.
HPV vaccines cannot protect against all types of HPV. If you are a woman and have received HPV vaccinations, you should still attend cervical screening (smear tests) as the vaccines do not guarantee that you will not develop cervical cancer in the future.
If you’re worried you may have an STI, visit your local GUM or sexual health clinic for advice.
You can find your nearest sexual health clinic by searching by postcode or town.
www.nhs.uk/Service-Search/Sexual-health-services/LocationSearch/1847
For information on all sexual health services, visit the FPA website below.
www.fpa.org.uk/where-get-help/sexual-health-helpline
*We would always recommend using a condom
Source NHS Choices